The new Urticaria Guideline
– What does it bring for patients?
Preface
This brochure is written for patients with urticaria, in order to describe relevant information included in the international urticaria guideline in a way that is easily understood by anyone. This is neither another guidebook nor another translation of the newest Urticaria Guideline. The Urticaria Guideline is written for doctors who need to understand exactly how and why they are to follow specific procedures when treating patients. For this reason, the Urticaria Guideline contains passages in which recommendations are made based on newest research results. These passages are also explained in this brochure, so that they can easily be understood by anyone. The original Urticaria Guideline was published in English in April 2014 and is available here: http://www.ga2len.net/PDF/Guideline.pdf. The structure of this brochure follows the same pattern as the Urticaria Guideline, so that the two can be read simultaneously.
Click on the headlines below to open the next chapters.
Medical guidelines are documents that meet specific requirements in order to enable doctors to make the right decisions. The treatment recommendation within the Guideline is based on scientific research and is practice-oriented. The current Urticaria Guideline was written and approved during a congress in Berlin in 2012, with the help of over 200 urticaria specialists from 39 countries. Prior to the congress, an expert panel had come up with related questions and sighted the most recent literature on urticaria. 188 publications were evaluated and 67 of them are included in the Guideline. All publications were evaluated according to the standardized GRADE (Grading of Recommendations Assessment, Development and Evaluation) system. In the evaluation process, levels of evidence were given to show to which degree the scientific evidence of these publications is weighed. The highest degree of evidence of a publication is reached by those publications that include multiple high-quality clinical trials. The lowest degree of evidence is awarded to case reports and expert opinions. If there was no literature whatsoever available for a question posed by the expert panel, the urticaria specialists had the option of choosing “clinical consensus”. Taking evidence and the opinion of those present into account, a consensus was reached in regards to the weight of the diagnostic and therapeutic questions (from “strongly recommend” to “recommended” and to “recommendation open”).
In the following text, you will find multiple text boxes, which contain the questions formed by the expert panel as well as the answers to those questions, using the method explained above.
Wheals and angioedema occur when specific skin cells (mast cells) are activated. Mast cells are the “fire department” or “border patrol” of the human body. Mast cells are abundant in those areas of the body that have immediate contact with our surroundings. This means that mast cells are not only found in the skin, but also in the mucus membrane of the gastro-intestinal tract and the airways. In this area, mast cells are vital to our health, as they recognize bacteria and parasites and keep them from doing harm. In the case of urticaria however, mast cells are activated without any exterior threat. Inflammatory substances such as histamine are being released. Histamine causes the blood vessels of the skin to expand, which causes swelling, reddening and itching of the skin.
Urticaria is class-divided into groups according to two characteristics. One group is characterized by urticaria symptoms that are acute (lasting less than six weeks) and the other group is characterized by chronic symptoms (lasting more than six weeks). The chronic form of urticaria is divided into either chronic spontaneous urticaria or chronic inducible urticaria. Symptoms of chronic inducible urticaria can be specifically evoked by certain stimuli and only appear when this stimuli is present. For physical urticaria, the largest group of inducible urticaria, these stimuli may be friction, cold, warmth, light or pressure. When the skin is exposed to these stimuli, the effect is wheals and/or angioedema. Another form of inducible urticaria is contact urticaria, in which certain substances cause wheals, for example, if the skin is exposed to stinging nettles or contact with a substance that one is allergic to. With all other inducible urticaria forms (other than the cholinergic urticaria) wheals are usually limited to the area of the skin that came in contact with the stimuli. The distribution of wheals is therefore not accidental, but rather corresponds to a pattern that implies what the stimuli may be. In the case of solar urticaria for example, wheals only appear on the skin exposed to light, whereas the skin not exposed to the light is completely free of symptoms. In the case of cholinergic urticaria, a common form of inducible urticaria, perspiration leads to wheals. Here, the reason for sweating is irrelevant, be it physical effort or a hot bath.
As opposed to the above-mentioned inducible forms of urticaria, wheals and angioedema appear arbitrarily in the case of spontaneous urticaria. The skin variations of the skin appear anywhere on the skin and the distribution and definition of wheals is random. Stress and warmth can cause the development of wheals and angioedema, but are not necessarily required to cause symptoms. In some cases, a patient suffers from two or more forms of urticaria at once. The frequency of the different types of urticaria is highly variable. By far, the most common form of urticaria is acute spontaneous urticaria. Approximately one in four people suffers from this form of urticaria at one point in their life. Luckily, these symptoms disappear on their own in many cases, sometimes within only a few days or weeks. The majority of patients with chronic urticaria suffer from chronic spontaneous urticaria. Less common are the inducible forms of chronic urticaria. In this group, most patients suffer from symptomatic dermographism (also known as dermographic urticaria or urticaria factitia), cholinergic urticaria, cold urticaria or contact urticaria. Aquagenic urticaria (triggered by water) or vibration induced angioedema are absolute rarities. In the following table all forms of urticaria are listed according to the previously mentioned criteria.
Table 1
Chronic | |
Chronic spontaneous urticaria (very frequent) | Chronic inducible urticaria (frequent) |
Spontanous appearence of wheals or angioedema or both for more than six weeks due to known or unknown causes | Physical Urticaria Symptomatic dermographism1 (frequent) Cold urticaria2 (frequent) Delayed pressure urticaria3 (rare) Solar urticaria (rare) Heat urticaria4 (very rare) Vibratory angioedema (very rare) Cholinergic urticaria (frequent) Contact Urticaria (frequent) Aquagenic urticaria (very rare)
1also known as urticaria factitia or dermographic urticaria; 2also known as cold contact urticaria; 3also known as pressure urticaria; 4also known as heat contact urticaria. |
Should the current classification be maintained in urticaria? We recommend to use this updated version of the classification2013 revision (strong recommendation/clinical consensus). |
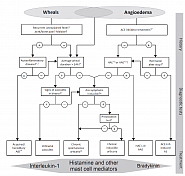
As wheals and angioedema can also be symptoms of other diseases, it is of high importance that other diseases are ruled out in each individual case, as these diseases are treated completely differently than urticaria. Such diseases include mastocytosis, urticaria vasculitis, or other different inflammatory diseases, all of which are characterized by wheals or wheal-resembling skin lesions, or also hereditary angioedema or ACE-inhibitor induced angioedema, which are all characterized by swellings. The guideline contains a chart that assists in ruling out other diseases than urticaria.
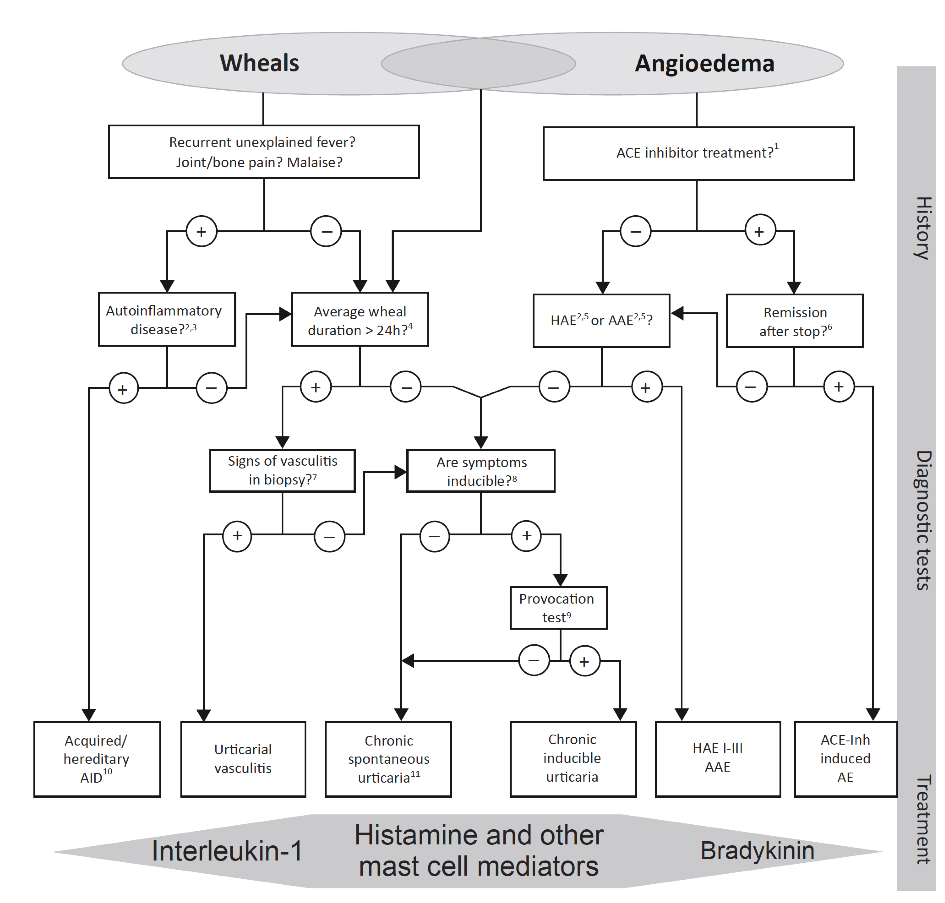
Diagnostic algorithm for patients presenting with wheals, angioedema, or both. AAE, Acquired angioedema due to C1-inhibitor deficiency; ACE-Inh, angiotensin-converting enzyme inhibitor; AID, Auto-inflammatory disease; HAE, Hereditary angioedema.
1Other (new) drugs may also induce bradykinin-mediated angioedema. 2Patients should be asked for a detailed family history and age of disease onset. 3Test for elevated inflammation markers (C-reactive protein, erythrocyte sedimentation rate) 4Patients should be asked: ‘How long do your wheals last?’ 5Test for Complement . 6 Wait for up to 6 months for remission; additional diagnostics to test for C1-inhibitor deficiency should only be performed, if the family history suggests hereditary angioedema. 7 Does the biopsy of lesional skin show urticarial vasculitis)? 8Patients should be asked: ‘Can you make your wheals come?’ 9In patients with a history suggestive of inducible urticaria, standardized provocation testing should be performed. 10Acquired autoinflammatory syndromes (AIDs) include Schnitzler’s Diasease and others. 11In some rare cases, recurrent angioedema is neither mast cell mediator mediated nor bradykinin-mediated, and the underlying pathomechanisms remain unknown. These rare cases are referred to as ‘idiopathic angioedema’ by some authors.
For doctors, it is important to have the means to measure the severity of a spontaneous urticaria. Only then is it possible to determine if the disease activity (symptoms) decreases or not with treatment. Decent treatment of diabetes, for example, would not be possible without measurement of the patient’s blood sugar. There is, unfortunately, no blood value that can give this information about the current status of a patient’s urticaria. The information about disease activity can only be collected by the patients themselves. In order to collect and evaluate this information in a structured way, different questionnaires have been developed for patients and the use of these questionnaires is highly recommended in the Guideline. At the time the Guideline was developed, the only measurement for the activity of spontaneous urticaria was the UAS7 (urticaria activity score). The number seven pertains to the seven consecutive days that the questionnaire is filled out. The UAS7 questions daily the severity of symptoms: 1) Number of wheals 2) Degree of itch (see table 2). The answer options are given a score value between 0 and 3, where 0 means that no wheals and no itch, respectively, were present. If the score of 3 is given, it means that the severity of symptoms is at an absolute maximum. The single value of “wheal” and “itch” are summarized.
Table 2
| Score | Wheals | Itch |
| 0 | None | None |
| 1 | Less than 20 wheals | Little |
| 2 | Between 20 and 50 wheals | Middle |
| 3 | Over 50 wheals | Strong |
The UAS value of a day can therefore lie between 0 (no symptoms) and 6 (over 50 wheals and strong itch). Due to the fact that the symptoms of urticaria are not constant but rather highly variable over time, information is entered into the UAS throughout the course of a week in order to record the varying degrees of the symptoms. The daily values are summarized so that the UAS7 score lies between 0 and 42.
For patients who also, or only, suffer from angioedema, the AAS (Angioedema Activity Score) is used, as this instrument is specifically designed to document angioedema and the correlating symptoms. The AAS is filled out every day over the course of four weeks. To measure the degree of inducible urticaria symptoms, it is best to measure a patient’s threshold for the trigger. In the case of a patient suffering from cold urticaria, for example, the highest temperature would be measured at which the symptoms are just barely brought about.
Should the current activity score (UAS7) be maintained assessing severity in urticaria? We recommend to use the UAS7 to assess severity (strong recommendation/clinical consensus). |
Urticaria can impair the patient´s quality of life considerably. According to the symptoms, several aspects of the quality of life can be affected. In the recent years, quality of life questionnaires were developed specifically for chronic urticaria (CU-Q2oL, Chronic Urticaria Quality of Life Questionnaire) and angioedema (AE-QoL, Angioedema Quality of Life Questionnaire). These questionnaires assess various facets of quality of life, including physical, emotional, social, and also practical aspects. These psychometric characteristics make them suitable for the assessment of the health burden of patients with chronic urticaria and angioedema.
Quality of life should be assessed before the initiation of a treatment and subsequently in regular intervals. The improvement of the patient´s quality of life is a major goal of the treatment. Only when the treatment outcome can be evaluated, the further treatment can be adapted and optimized accordingly.
Which instrument should be used to measure QoL in urticaria? We recommend using the validated CU-Q2oL and AE-QoL instruments for assessing QoL impairment and to monitor disease activity (strong recommendation/clinical consensus). |
In the last two decades, great progress was made in researching the causes of urticaria. The causes of chronic spontaneous urticaria can be divided into three broad groups: Autoreactivity, intolerance to certain foods or medicine and infectious diseases.
Autoreactive urticaria: In the case of autoreactive urticaria, the body produces substances that are released into the blood stream, which activate mast cells when these substances reach the skin. An example of this is the so-called autoimmune urticaria, in which the immune system of the body produces antibodies (immunoglobulin) against the body’s own proteins. The antibodies then attack the proteins as if they were dangerous intruders, such as bacteria. In this case, the body is basically fighting itself. This is why antibodies are also called autoantibodies. Often autoantibodies against IgE (allergy antibody) or the IgE receptor are found in patients with autoimmune urticaria. If these autoantibodies encounter IgE that has docked on to mast cells (or the receptor of the mast cell), the mast cell is stimulated and releases histamine which causes wheals and itch. Autoreactive urticaria is diagnosed easily, quickly and effectively with the help of the autologous serum test (ASST = autologous serum skin test). In order to do this, serum from freshly acquired whole blood is injected into the patient’s skin in a type of allergy test. If a wheal results, this shows that the patients are “allergic” to their own serum.
Intolerance urticaria: Patients with chronic spontaneous urticaria often suspect that their symptoms correlate with the consumption of certain foods, but allergy tests are found to be negative. This indicates an intolerance urticaria. This form of urticaria is not a result of a “real” allergic reaction to food, but a dose-related and delayed (four to twelve hours) intolerance to so-called pseudo allergens, for example a dye, a preservative, an aromatic substance or a natural food component. The exact mechanisms that lead to mast cell activation in intolerance urticaria are still unknown.
Infectious urticaria: It has long been known that chronic spontaneous urticaria can result from infectious processes. It is assumed by extension that misdirection of the immune system in the defense against infections is the cause. Especially infections in the gastro-intestinal area due to helicobacter pylori and infections in the throat-nose-mouth area or the dental root are quite frequently the cause of an infectious urticaria.
The frequency of the single causes of chronic spontaneous urticaria is not easily defined, as the literature on this topic reflects regional differences, such as nutrition or the frequency with which certain infectious diseases exist in a certain region, and this leads to varying results in causes. In the inducible forms of urticaria, the underlying causes are almost always unknown. Neither autoreactive urticaria nor intolerance actions seem to play an important role, merely infectious diseases can be the cause in individual cases.
During the initial patient visit, a thorough history, including the patient’s medical history, should be taken. The physician should ensure that the following is considered:
- Time of onset of disease
- Frequency/duration of and provoking factors for wheals
- Variations in daily routine
- Occurrence in relation to weekends, holidays and foreign travel
- Shape, size and distribution of wheals
- Appearance of angioedema
- Associated symptoms, such as itch and pain
- Family and personal history regarding urticaria and allergies
- Previous or current allergies, infections, internal diseases or other possible causes
- Psychosomatic und psychiatric diseases
- Surgical implants and events during surgery, for example after local anesthesia
- Gastric/intestinal problems
- Induction of symptoms through external physical agents or exercise
- Use of drugs (e.g., non-steroidal , auto-inflammatory drugs (NSAIDs), injections, vaccinations, hormones, laxatives, suppositories, ear and eye drops and alternative remedies
- Correlation to food
- Correlation to menstrual cycle
- Smoking habits (especially the use of perfumed tabacco products or cannabis)
- Type of work
- Hobbies
- Stress
- Quality of life in relation to urticaria and emotional impact
- Previous therapy and response to therapy
- Previous diagnostic procedures/results
Subsequent diagnostic steps depend on the subtype of urticaria diagnosed as well as the results of the history. In the case of an acute urticaria, a diagnostic workup is highly advised against, as the spontaneous cure rate of acute urticaria is so high, that most patients are free of symptoms before the results of the medical exam are received.
Should routine diagnostic measures be performed in acute urticaria? We recommend against any routine diagnostic measures in acute urticaria (strong recommendation/clinical consensus). |
Should routine diagnostic measures be performed in chronic spontaneous urticaria? We recommend for only very limited routine diagnostic measures in chronic spontaneous urticaria (strong recommendation/ clinical consensus). |
Should extended diagnostic measures be performed in chronic spontaneous urticaria? We recommend for only limited extended diagnostic measures in chronic spontaneous urticaria based on patient history (strong recommendation/clinical consensus). |
Should routine diagnostic measures be performed in inducible, non-spontaneous subtypes of urticaria? We recommend limiting routine diagnostic measures to determining the threshold of eliciting factors in inducible urticaria subtypes (strong recommendation/clinical consensus). |
In chronic spontaneous urticaria, the guideline recommends limiting the search for an infectious disease as the underlying cause to a blood test (blood count, inflammation values and erythrocyte sedimentation rate or C-reactive protein). Only if the result of this test, or the patient’s medical history, strongly indicates an underlying cause, should further tests be considered:
- Thorough diagnostic assessment of inflammatory causes
- Allergies
- Thyroid problems
- Skin tests/testing the functionality of the skin
- Diet low in pseudo allergens
- Tryptase (a mast cell enzyme that can be measured in the blood)
- Autologus Serumtests (ASST)
- Biopsy of the skin
The recommended tests for all forms of inducible urticaria are limited to confirmation of urticaria and, if applicable, to measuring the threshold for the relevant trigger by use of a challenge test. In such a challenge test, the skin of the patient is confronted with different strengths of the trigger and the reactions of the skin are documented. Challenge tests are available for use in patients with cold urticaria, heat urticaria, symptomatic dermographism, solar urticaria, and pressure urticaria, in addition to other standardized instruments or methods. The Guideline also recommends the development of such instruments or methods for the other types of urticaria.
A routine screening for malignant tumors is not recommended. Blood tests of chronic spontaneous urticaria patients often show decreased levels of specific white blood cells, the basophils. The relevance of this observation is unclear. The authors of the guideline call for more research to be done in this field.
People of any age can suffer from urticaria. Children suffer comparatively more frequently from an acute spontaneous urticaria. Virus infections and food incompatibilities seem to be predominant stimuli for children who suffer from urticaria, as opposed to food allergies in adults. If a food allergy is suspected, this should be extensively pursued. As other causes for urticaria in adults and children vary very little in all other areas, the same diagnostic approach can be used for children (other than infants) as for adults.
General Considerations
- With the exception of acute spontaneous urticaria, urticaria is a chronic disease. Symptoms of urticaria are caused by mast cell activation, which releases substances into the skin, most of all histamine, which causes the skin to react with itching, wheals and angioedema. While diagnostic methods must differentiate between the different urticaria sub-types, the treatment of the different forms of urticaria and urticaria sub-types are quite consistent. As with other mast cell related diseases, a general concept of treatment is recommended: a) eliminate stimuli or cause, b) block mast cell activation and mast cell active substances, and c) if possible, inducing tolerance treatment.
- Depending on the type of urticaria or the combination of different sub-types that a patient suffers from, symptoms can either appear continually or in spurts, spontaneous or induced. This reaction pattern must be taken into consideration when choosing the appropriate therapy.
- As acute urticaria is defined by very short duration of symptoms, medical treatment of symptoms should be symptomatic.
Should the treatment aim at complete symptom control in urticaria? |
The requirement to successfully avoid specific stimuli is determined by how exact the diagnosis is. Generally, the determination of stimuli in inducible urticaria is quite successful; however, determining the stimuli for chronic spontaneous urticaria is not always as easy. If a patient suffers from an infectious disease for example, this could be the cause for urticaria as well as the cause for more severe symptoms. However, it is also possible that it could simply be chance that the patient suffers from both and one is not related to the other. In this case, the inflammatory disease would have to be eliminated and only then would it be possible to determine if the urticaria symptoms lessen or not. Should the urticaria symptoms improve in this case, it is also possible that this was spontaneous remittance. Should the suspected stimuli be a certain medication or type of food and the symptoms vanish after avoiding the suspected stimuli, it can, in some cases, be worth taking a provocation test. In this case, the patient is confronted with the suspected stimuli in a monitored environment. If the symptoms occur in this situation, this would serve as evidence for correlation between symptoms and stimuli.
If medication is the suspected stimuli for urticaria, the patient should no longer take the medication (or in most cases, take an alternative medication made from different substance matter). The most known medical substances that are known to cause urticaria are pain relievers, so called nonsteroidal anti-inflammatory drug. Typical medications with these substances are ASS (acetylsalicylic acid) Ibuprofen or Diclofenac. These medications are not only known to cause urticaria, but can also worsen the symptoms of an already present urticaria. Completely avoiding these substances does not always guarantee complete freedom of symptoms.
In the case of physical urticaria, avoiding the stimuli is recommended. The prerequisite for this, is of course, knowing the exact stimuli, which is almost always possible in the case of a thorough diagnosis. Avoiding physical stimuli in day-to-day life can be very challenging. No one is able to entirely avoid pressure. Patients with pressure urticaria need to do exactly this. To enable patients to do this, one must understand that pressure is a combination of surface area and strength. Where pressure itself cannot be avoided, it can be decreased if the surface area is increased. Consider a purse, for example. If the strap of the purse is widened to double the previous width, then shoulder on which the strap lays is only subjected to half of the pressure as it would be with the more slender strap. Similarly, patients with solar urticaria need to know to which wavelength of the light they react, in order to adjust light and sun protection adequately.
Chronic illnesses are often found to be the reason for chronic spontaneous urticaria: In physical urticaria this reason is only found in a few cases of cold urticaria and symptomatic dermographism. The cause for the above is often known to be infections on the gastro-intestinal tract (bacterial or parasitic) as well as those in the throat-nose-mouth area. Research results show varying results to correlation and frequency of chronic spontaneous urticaria and an infection with helicobacter pylori. Helicobacter pylorus is a bacterium that settles in the human stomach and causes gastritis. Gastritis, such as other chronic inflammations, does not always go hand in had with specific symptoms or pain. However, it is always the case that the body always confronts these “invaders” with the body’s own immune system. The immune system’s reaction to the helicobacter pylori can, in some cases, cause urticaria. This is why it is recommended to eliminate the infection/inflammation, and this can generally be done with relevant antibiotic treatment.
In the past, patients suffering from autoimmune urticaria have profited from having their blood cleaned. However, this is a very costly form of therapy and there is not much experience with this form of therapy as treatment to date.
Real immediate food allergies (for example in the case of a peanut allergy) are almost never the cause of a chronic spontaneous urticaria. If urticaria is related to food, it is generally a reaction which is unspecific, delayed and dependent of to the amount of ingested food. Several nutritional ingredients such as food coloring, aromatics or preservatives can cause a chronic spontaneous urticaria or worsen already present symptoms. These substances can be of artificial or natural origin, such as fruits and vegetables. Avoiding these certain substances (the so-called pseudoallergen-free diet) can lead to a reduction of symptoms in two to three weeks. As treatment, this diet should be adhered to for three to six months. It must be mentioned that the responses in success rate of this therapy varies greatly from region to region and may therefore be related varying cultural eating habits. This is an area that still needs much research.
Should patients with an allergic sensitization (positive specific igE/skin prick test) avoid certain food items? We recommend that patients with a known sensitization based on specific IgE to food should only avoid these foods if there is relevant information e.g double blind oral provocation test or a clear history, to prove that the sensitization has a clinical relevance for urticaria (strong recommendation/high level of evidence). |
Are pseudoallergen-free diets useful in the extended diagnostic program of chronic spontaneous urticaria? |
Inducing tolerance is generally possible for different types of inducible urticaria. A general improvement of symptoms has been reported after repeated confrontation with the stimuli in regard to cold urticaria, symptomatic dermographism, solar urticaria, and cholinergeric urticaria. Alleviation of symptoms with this method only lasts a few days, which is why this therapy must be continued.
Symptomatic treatment means treating the symptoms of a disease. The difference between this and a causal therapy is that in this case, the underlying cause for the disease is not treated, but rather the symptoms are. This is why symptomatic treatment does not generally have an effect on the course of the disease. Symptomatic therapy is the most important use of therapy for chronic urticaria and aims to neutralize the mast cell mediators, most of all that of the histamine. This is what antihistamines are for, such as: cetirizine, levocetirizine, loratadine, desloratadine, rupatadine, fexofenadine or ebastine. These antihistamines block the so-called H1 histamine receptor on blood vessels and nerves. H1 histamine receptors are almost only found in the skin. Taking this medication continuously is recommended in order to achieve best possible results.
Aside from histamine, other mast cell mediators play a role in chronic spontaneous urticaria as well, such as PAF, leukotrienes and cytokines. There is medication that can block the PAF and also some that can block the leukotrienes. Older antihistamines have the predominant disposition of making the central nervous system drowsy, and this drowsiness lasts longer than the reduction of itch. In addition, these medications have an effect on the sleep-cycle, which can then have a negative effect on the patient’s overall performance. Therefore, the Guideline strongly advises against the use of these older forms of antihistamines, which cause drowsiness, and instead strongly recommend the use of modern, non-drowsy antihistamines when treating chronic spontaneous urticaria. This recommendation is based on multiple studies that show that these modern antihistamines are not only more effective, but also have fewer side effects. The side effects of older antihistamines are by now understood quite well. The medication overrides the blood-brain-barrier and binds the H1 receptors of the central nervous system, where they interfere with the neurotransmitter effects of histamine. The effect on activities that involve multi-tasking and tasks involving complex sequences of motion, such as driving, are very strong.
Old first-generation H1-antihistamines are a particular concern in the elderly in whom they increase the risk of impaired cognition, inattention, disorganized speech, altered consciousness, and falls. The development of the modern, second-generation antihistamines led to medication that has very few or no drowsiness causing side effects. Two of these new developments, astemizole and terfendadine, show increased side effects when taken with a certain antibiotic or a certain antifungal drugs. That is why these two medications are no longer on the market in most countries. Many of the modern antihistamines are slight variations or metabolic products of other antihistamines. Not all antihistamines were tested extensively for their effects on urticaria, comparative studies between different antihistamines in particular are scarcely available. In total, however, there are ample clinical studies that prove the effect and safety of modern antihistamines, which is why this is the therapy of choice.
Are modern second generation H1-antihistamines to be preferred over first generation H1-antihistamines in treatment of urticaria? We recommend that modern second generation H1-antihistamines are to be preferred over first generation H1-antihistamines in the treatment of urticaria (strong recommendation/high level of evidence). |
Multiple other studies show that modern antihistamines, given in a higher dose than expert product summary suggest, work well in improving the symptoms of urticaria without influencing the safety of the patient. Such studies have been made for: cetirizine, levocetirizine, desloratadine, rupatadine, fexofenadine and bilastine. All of these studies showed that the majority of urticaria patients that adhered to the recommended dose and did not react greatly, profited from a higher dose of antihistamine. Due to this data, the Guideline recommends modern antihistamines in a simple dose as the preferred therapy, and in a higher dose as the therapy for second choice.
Is an increase in the dose to the fourfold of modern second generation H1-antihistamines useful as second line treatment and to be preferred over other treatments in urticaria? We recommend a trial of up to fourfold dose of modern second generation H1-antihistamines as second-line in the algorithm of treatment. |
Should modern second generation H1-antihistamines be taken regularly or as needed? |
Should different H1-antihistmanies be used at the same time? We recommend preferably to updose modern second generation oral H1-antihistamines to be taken continuously in the lowest necessary dose rather than on demand (strong recommendation/high-quality evidence). |
If there is no improvement, should higher than fourfold doses of H1-antihistamines be used? |
1. Modern non-sedating antihistamines in single dose | |
| ↓ If symptoms persist after two weeks | |
2. Increase dosage up to fourfold of modern non-sedating anti-histamines | |
| ↓ If symptoms persist after one to four further weeks | |
3. In addition: Omalizumab, Ciclosporin A or Montelukast |
First choice therapy is antihistamines in with regular doses.
This recommendation is supported by excellent data collected from many studies. Low costs and wide availability worldwide of antihistamines ensures safe and successful treatment.
Second choice therapy: Also here there is supportive data collected from multiple studies. Low costs, effective and safe treatment.
Third choice therapy in addition to antihistamines:
- Cyclosporin A:
Ample data from supportive studies, middle to high costs, moderate safety profile, good results. - Omalizumab:
Very good data from supportive studies, high costs, very safe and a good success rate for treatment - Montelukast:
Little supportive data from studies, low costs, quite safe and low success rate for treatment - Cortisone as short-course treatment
Few studies, low-costs, worldwide availability, quite safe if used for short periods of time and good success rate for treatment
Omalizumab is a so-called biological. Biologicals are proteins manufactured in biological sources that specifically intervene in a function of the body. In the case of Omalizumab, this protein is a so-called antibody, a defending substance that specifically neutralizes the allergy protein IgE in the body. It is not extensively researched, as of yet, as to why the reduction of IgE in the body leads to a much decreased activation of mast cells. Omalizumab was originally developed to treat allergic asthma; and in recent years, it has shown to be a very effective therapy for the different forms of urticaria. When the guideline was published, Omalizumab was not yet approved for treatment. Omalizumab has now been approved for chronic spontaneous urticaria, in cases where patients do not respond to antihistamines.
Is Omalizumab useful in the treatment of patients unresponsive to high doses of H1-antihistamines as third-line treatment? We recommend a trial of Omalizumab as add on therapy to modern second generation H1-antihistamines as third-line in the algorithm of treatment of urticaria (strong recommendation/high level of evidence). |
Cyclosporine A is a drug substance that belongs to the group of immunosuppressants that are mostly used for patients with organ transplants, as they prevent the new organs from being rejected. Cyclosporine A also has the direct effect that it releases mast cell mediators. Controlled studies show success of treatment for urticaria with a combination of Cyclosporine A and antihistamines. Due to the multiple side-effects of Cyclosporine A, it is not recommended for use as standard therapy. Nonetheless, these side effects are still far less than that of a long-time cortisone therapy. This is why this should only be considered for patients that do not respond to antihistamines at all.
Is ciclosporin A useful as add on treatment inpatients unresponsive to high doses of H1-antihistamines as third-line treatment? We recommend a trial of ciclosporin A as add on therapy tomodern second generation H1-antihistamines as third-line in the algorithm of treatment of urticaria (strong recommendation/ high level of evidence). |
Research on the use of leukotriene antagonists was done in older studies. Leukotrienes are substances that are set free when mast cells are activated, and these substances also support the inflammatory reaction of an urticaria. Some of these studies showed that this therapy has some effect on urticaria. The studies themselves are hard to compare, due to the varying groups of patients included in the studies. The most effective of these seem to be Leukotrien-antagonist montelukast for urticaria.
Should leukotriene antagonists be used in the third line treatment of urticaria? |
While cortisone creams are very successfully applied in other forms of allergic diseases, they are of no use when it comes to urticaria. Systemically given cortisone, as pill or via injection, suppresses the symptoms of urticaria very effectively if the daily does lies between 20 mg and 50 mg, but such regularly given high doses, side effects are inevitable. This is why use long-term cortisone treatment is highly advised against. Short-term systemic application, can however, be considered for acute urticaria or for treatment for symptom flare. This treatment should not last more than ten days.
Should oral corticosteroids be used in the treatment of urticaria? and We suggest a trial of a short course of systemic corticosteroids in urticaria as third-line therapy or as an option for acute exacerbation (weak recommendation/low level of evidence). |
Increasing the dose of antihistamines, up to fourfold the recommended dose, generally helps most urticaria patients. For those, however, that do not respond to this treatment, alternative treatments must be used. Patients should be sufficiently treated with antihistamines to ensure full effect potential is reached. A time period of one to four weeks is recommended for treatment with high doses of antihistamines, to accurately assess the effectiveness of the treatment. The severity of urticaria can vary greatly over time and spontaneous remission is possible at any time. Therefore, the need to maintain or adjust treatment should be checked every three to six months. There is not much data available in regard to how medications are, or should be, combined in the treatment of urticaria. The most data available concerns the use of antihistamines and omalizumab or cyclosporine. Less research has been done on the combination of antistamines and leukotoriene antagonists. This is why the recommendation in the third step of the therapy algorithm is very limited. The combination of antihistamine and dapsone was recommended in the last Guideline, however, the data available was unsatisfactory and therefore this recommendation was not included in the therapy algorithm. In some health systems with limited resources, this combination still has a standing value. Other therapy options were researched in small-scale studies in the past, yet due to the quality of these studies, no general recommendation for treatment arose from them. Medication that may have possible effects but cannot be directly recommended include:
sulfasalazine, methotrexate, interferon, plasmapheresis, phototherapy, and intravenous immunoglobulins (IVIG) such as TNF-Alpha-Inhibitors. Some treatments that were used earlier on and that were thought to alleviate symptoms have been found to be ineffective. These methods should no longer be used. These include:
tranexamic acid, sodium cromoglicate, nifedipin, colchicine, indomethacin. It is possible that some of these therapy forms must be put to the test again, as it is not definite that they cannot be of effective use for some sub-groups.
Children
Many practitioners use old treatment methods when treating children, such as first-generation antihistamines, as they assume that this safety profile is better known than that of modern, second-generation antihistamines. Second-generation antihistamines are not approved for use for children under the age of six months, whereas first-generation antihistamines have fewer restrictions for use. It is important to consider the fact that these antihistamines were approved for use when regulations for medicine approval were more lenient. As a result of this, many practitioners continue using the first-generation antihistamines, which actually, as shown above, have less of a security profile than those that have more recently been developed. The Guideline highly advises against the use of these first-generation antihistamines when treating children or infants. It is recommended to use the same therapy for children as for adults. An increase of dosage in regard to antihistamines should be in correlation to the weight of the patient. When treating children, only antihistamines that have been extensively tested should be used for therapy. The following antihistamines have been extensively tested in studies with children and also include long-term safety: cetirizine, desloratadine, fexofenadine, levocetirizine and loratadine.
The antihistamines used for treatment need to be chosen on an individual basis. This depends on the age of the child and the antihistamines available for treatment. Not all of the above mentioned antihistamines are available in all countries in the form of drops, juice or quickly dissolving tablets.
Should the same treatment algorithm be used in children? We suggest the same treatment algorithm be used in children with chronic spontaneous urticaria (weak recommendation/clinical consensus). |
Pregnant and nursing women
The same considerations as above also apply for pregnant and nursing women. On one hand, any systematic treatment in the first trimester should be avoided, on the other hand, expecting women also have the right for the best possible therapy. The safety of medication during pregnancy was not systematically researched. However, it must be mentioned that the possible negative effects of higher histamine values, which are prevalent in the case of urticaria, have also not been extensively researched. As of date, no birth defects have been reported when modern antihistamines were used for treatment during pregnancy. There is only a small observatory study for cetirizine and a large one for Loratadine, which show this. In addition, some of the modern antihistamines can be obtained without prescription and have been widely used for years in treatment of hay fever and urticaria, so that it can be assumed that many women took these medications, especially early on in their pregnancy. As the highest safety standards are to be considered in the case of pregnant women, it is recommended to use loratadine and cetirizine, and considering the possible use of closely related desloratadine and levocetirizine. All H1 antihistamines are excreted in the mother’s milk in minimal doses. This is why the use of second-generation, non-drowsy antihistamines is highly recommended, in order not to transfer the side effects of drowsiness to the infant. The recommendation of increasing the dose of antihistamines during pregnancy is given with certain reservation, as there are no studies about the safety of this. In the case of the patient not responding to modern antihistamine treatment, the use of first-generation antihistamines can be considered in individual cases. The uses of these first-generation antihistamines right before birth can, however, effect the newborn. All further steps of therapy must be considered on an individual basis and in respect to the risks and side effects on mother and child.
Should the same treatment algorithm be used in pregnant women and during lactation? We suggest the same treatment algorithm be sued in pregnant women and during lactation in urticaria (weak recommendation/clinical consensus). |
The authors of this guideline express the necessity for further research in the following areas:
- Frequency of illness in adults and children
- The social and economic consequences of the illness
- Further research done on activating factors of mast cells
- Histological markers
- Research of blood values that correlate to urticaria activity
- Research done using the questionnaires of urticaria activity and quality of life
- Research about the role of coagulation factors in chronic spontaneous urticaria
- The development of tests that demonstrate the presence antibodies against IgE or the IgE receptor
- Research done in regard to psychological illnesses related to urticaria
- Particularities of forms of urticaria resistant to antihistamines
- Studies that compare the modern antihistamines to each other, especially in higher doses and with the different forms of urticaria
- Studies that compare the use of regularly administered antihistamines to the use of antihistamines administered during irregular intervals
- Large studies that research the possible effects of coagulate substances on urticaria
- Controlled multicenter trials on the possible effect of add-on of anti-H2, montelukast, sulfone, methotrexate, azathioprine
Urticaria | Also known as nettle rash, is the overall term to describe a group of illnesses that include symptoms of itching wheals and angioedema. |
Angioedema | A temporary swelling that lies deep within the tissue of the body. The cause of swelling is a shift of fluid from the blood, caused by a temporarily “leaking” of the blood vessels. This “leaking” is communicated through histamine. |
Histamine | A messenger substance that is stored in mast cells. Histamine causes the typical symptoms of urticaria: Wheals, angioedema, reddening and itch. |
Wheal | A temporary swelling in the top layers of the skin that looks like the burn of a stinging nettle. The cause of the wheal is a shift of fluid from the blood, caused by a temporarily “leaking” of the blood vessels. In the case of urticaria, this “leaking” is communicated through histamine. |
Clinical Study (Clinical trial) | Clinical studies are strongly regimented experiments that are made in order to test the effectiveness or safety of medication on healthy people or patients suffering from a certain illness. These studies are done to answer scientific questions and to improve medical treatment. |
Antihistamines | „Allergy pill“. The active substance of an antihistamine blocks the histamine receptors on the blood cells and nerves and thus prevents histamine from unfolding its effect (urticaria). |
Antileukotriene agents | Medication that is actually approved for treating asthma. The active substance of an antileukotreine agent blocks the leukotriene receptors and thus prevents the inflammatory reaction that is caused by the leukotrienes. To a minimal degree, leukotrienes can play a role in urticaria. |
Mast Cells | Mast cells are immune cells, which store messenger cells such as histamine. These cells are found in the skin, the intestines and airways. Mast cells can release their messenger cells quickly once activated. They are the key cells in causing urticaria and many other allergic illnesses. |
Tryptase | An enzyme that is almost only found in mast cells. The levels of tryptase in the blood allows for conclusions to be drawn for mast cell messenger illnesses in correlation to the number and activity of mast cells. |
Cyclosporin A | Medical substance in the group of immunosuppressives (inhibitors of the immune system). This medication is most commonly used patients with organ transplants in order to avoid organs being rejected by the body. It is also used for treatment of severe urticaria. |
Cortisone | Cortisone is a hormone which is naturally produced in the adrenal cortex of the human body. There are many variations of cortisone that are synthetically produced and used in the medical field to suppress hyperactive reactions of the immune system Although cortisone is naturally produced by the body, there are side effects when used over long periods of time, some of which can be severe. This is why cortisone is not recommended for use except for short periods of time (as a pill or given as an injection) if symptoms cannot be controlled otherwise. The use of cortisone creams as treatment are not of use for urticaria. |
HAE AAE
| HAE: Hereditary (Inherited) Angioedema AAE: Angioedema acquired through C1 inhibitor deficiency These two diseases can be confused with urticaria, as urticaria symptoms can also include recurring angioedema. The cause of these diseases is entirely different than those of urticaria, which is why HAE and AAE are treated entirely different. |